Simon Fraser University Engineering Science professor Dr. Mirza Faisal Beg was born in Bhopal, India. He had his B.Tech. in Instrumentation Engineering from the Indian Institute of Technology. He then completed his Ph.D. in Biomedical Engineering at Johns Hopkins University in Baltimore, USA, and his MS in Biomedical Engineering from Boston University. He has been involved in AI technology for the past 30 years.
Now, he spearheads research that could help redefine cancer treatment. Using artificial intelligence (AI), his breakthrough research enables imaging of the human body and organ measurements much faster than traditional methods, signaling a leap forward in harnessing AI for individually personalized healthcare solutions.
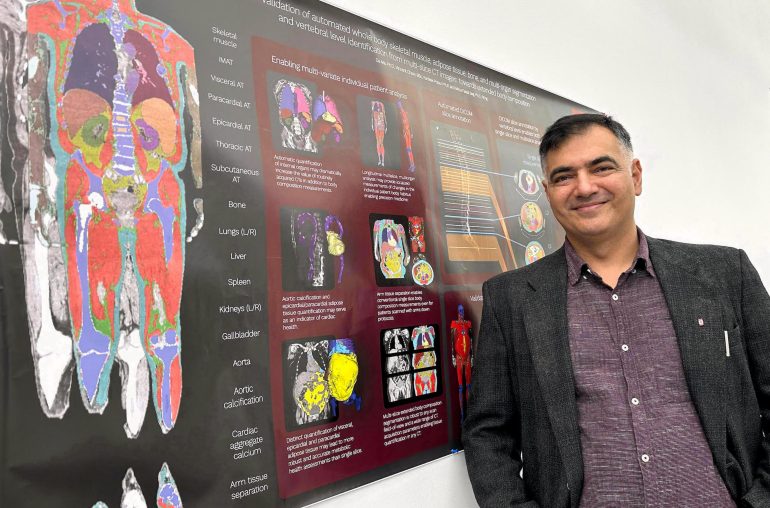
Beg and his team have created the Data Analysis Facilitation Suite (DAFS), a sophisticated, first-of-its-kind computer program delivering AI automation to provide measurements of many internal organs and tissues within the human body—in a matter of minutes.
The tool analyzes digital body CT scans and quantifies muscle, fat, and organ health. Rapid assessments offer insights into treatment responses, enabling tailored interventions and minimizing inadvertent side effects.
Dr. Beg says when treating cancer, there are two main steps. First, we find out how much the cancer has spread in the patient’s body. This helps decide the type of treatment needed. Second, we check the patient’s overall health. This tells us how strong a treatment they can handle.
Basically, the treatment depends on how advanced the cancer is and what the patient’s body can handle. For example, a young, strong patient might get a different treatment than an older, weaker patient. So, everyone’s treatment can be a bit different based on their health.
Dr. Beg explains, “Chemotherapy is a medicine that kills tumor cells that are growing fast. This helps to remove the cancer cells, but it can be tough on the body as it can also harm some healthy cells. So, doctors need to find the right balance.”
” Muscles can help protect against the tough effects of chemotherapy. A patient’s BMI measured using weight and height can give clues about their muscle amount. But there’s a problem: weight includes everything – muscles, fat, bones and all the other organs. So, two people might weigh the same but because of differences in other organs, they can have different amounts of muscle. Just relying on BMI might not tell the full story.”
“One way to see muscle is through CT scans. A full-body scan can give up to 1,000 images of the body. You can spot muscles in each image but measuring them by hand is tedious and takes forever. After a while, humans might even make mistakes because it’s boring to do the same thing again and again.”
“That’s where AI technology helps. Instead of humans spending countless hours measuring muscle, AI can do it in minutes. This saves a lot of time, letting doctors focus more on helping the patient.”
But—is it accurate?
“Dr. Beg says the AI works really well 95% of the time. But because our bodies are so complicated, the AI sometimes gets confused with 5% of the scans and those need some corrections. Think of the AI like a beginner medical student. It’s doing quite well, but it’s still learning from its mistakes. Over time, as we teach it more, it will get even better. Soon, it might become almost perfect at understanding medical pictures and spotting problems in them.
Right now, we don’t have many good ways to check how a patient’s organs are doing during treatment. But AI can look at medical pictures like CT scans to see and measure our organs. This helps doctors see if the treatment is working right. AI has improved a lot over 30 years and can help us understand changes in our body during different treatments.
Dr. Beg’s team is using AI to quickly measure the internal parts of our body. This can help doctors create a treatment plan that’s just right for each person, helping them get better while avoiding side effects.”
The innovation recently secured a Canadian Institutes of Health Research (CIHR) project fund to expand the team’s work and make its platform more accurate and comprehensive.
The team will continue to leverage the capabilities of AI in refining the pioneering technology to enable measurements of human body composition and their change due to disease and intervention that were not previously possible.
The goal of Dr. Beg’s research is to have treatments made just for you. He says, “We hope this technology can be used in clinics in the future to choose and custom design the treatments for each person. This means everyone can get the best possible treatment for their body. And with AI, this might happen even sooner.”