Why donate?
The truth runs deeper than the pride of writing a cheque, or the overall purpose of simply giving back. For the East to West Group, it’s personal.
In 2014, the three-year-old nephew of East to West Group’s Co-founder, Jag Sikham, was diagnosed with FSGS (formally known as focal segmental glomerulosclerosis). FSGS is a rare disease that can cause permanent kidney damage or even failure.
“It was heartbreaking to see a child so close to us go through something so devastating,” says Sikham. He has really inspired us to not take life for granted and to try our best to give back.

BC Children’s Hospital played a vital role. The family faced years of daily hospital visits for dialysis, bloodwork and follow-up appointments. Then came a heartbreaking failed kidney transplant in 2016. The disease was taking a toll on the young boy’s life both physically and mentally.
With the help of BC Children’s Hospital, the family decided to begin dialysis management in the comfort of the child’s home. This provided a certain sense of spontaneity, as well as a better quality of life.
Fast forward eight years after the initial diagnosis, and today you’ll find an 11-year-old boy living larger than life. His charismatic personality breaks through the daily obstacles of living with FSGS. Between the nightly dialysis, weekly appointments at the hospital and medications and their side effects—this pre-teen continues to play video games, do martial arts and keep his family laughing. There is also hope on the horizon that a successful transplant could send him soaring.
The sky is the limit
The connections between East to West Group and BCCH go beyond this one story. Many team members and clients have shared their experience of exceptional care and support from BCCH when their families needed it the most.
From pregnancy care to in-hospital births and special attention for other infant and childhood health concerns, BCCH has touched the lives of many people in the East to West Group family. Regardless of the reason for care, the support is always described as world class and invaluable.
“As our families, our staff and client base grow, we are exposed to more and more stories of children that currently use or have used resources at BC Children’s Hospital,” says Aman Bring, Co-founder.
And that drives the East to West Group team to do as much as possible to support the hospital. At the same time, the team is cultivating a deeper passion to give back.
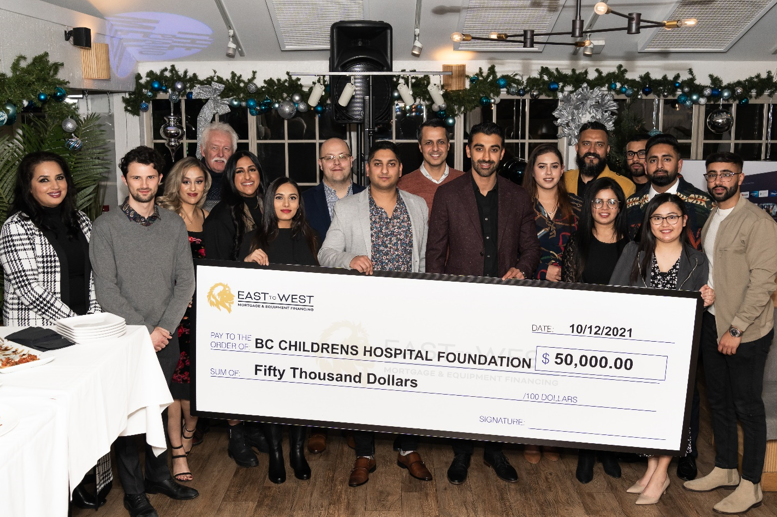
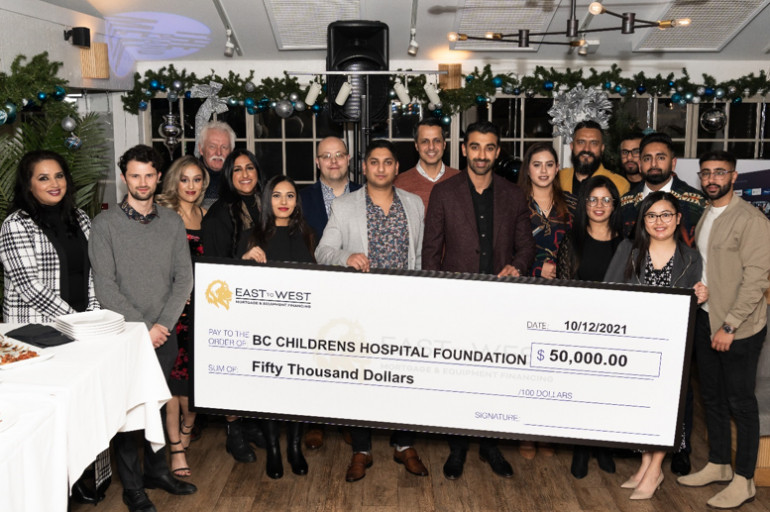
In 2021 alone, East to West Group donated $50,000 to the BCCHF. Overall, they’ve donated more than $100,000 spanning six years. The Co-founders encourage all businesses to give back to not only help the community, but also to boost team morale, and have a net positive social impact.
“We hit this goal sooner than we ever believed we could,” Aman Bring. “We owe a heartfelt thank you to our staff, clients, and lending partners for their support. The BCCH continues to play an essential role in many of our lives. We are grateful that we can come together and do our part to give back.”